|
Does Your Food Look Like and Taste Like Plastic? Here’s the Reason Why
Have you noticed that your meat is unnaturally rubbery, and your vegetables seem to bend, not break? This is a sign of a serious issue-they're contaminated with phthalates, a problem that's now at epidemic levels. The concerning part? Government regulations are lagging behind the mounting evidence of the health risks these phthalates pose. What Are Phthalates? Named the “forever chemical,” phthalates are plasticizers used to create durability, flexibility, transparency, and longevity in products that contaminate our foods. They are used in canned foods, infant foods, packaging, and sealants; they are everywhere. The government regulates a “safe” level, but that safe level does not seem to be consistent with current research on the levels that cause adverse health impacts. Where Are Phthalates Found? Foods highest in phthalates are:
What Are the Health Problems Associated with Phthalates? These eight plasticizers are all endocrine disruptors that have ill effects on reproductive health, childhood development, insulin resistance, the development of high blood pressure, obesity, breast cancer, allergy, asthma, and diabetes. The FDA has continually denied petitions from other groups to change the levels of plasticizers allowed in food products, even being sued once. However, despite years of protests, petitions, and lawsuits, the FDA refuses to change the levels they have deemed safe despite proof that such levels cause human harm. Reducing Your Exposure to Plasticizers Here are some action tips to reduce your level of contamination from forever chemicals.
It looks like plasticizers are here to stay, so just try to avoid them as much as you can. It is sad that we cannot depend on the FDA to protect us from known contaminants that cause human harm. After all, isn’t that one of their roles? Comment from Reader Per- and polyfluoroalkyl substances also known as "Forever Chemicals" are used in many chemical and manufacturing processes. Humans can be exposed to PFAS in the air, food, water, dust, soil, food wrappers, cosmetics and personal care products. PFAS have been associated with serious health effects including cancer, organ damage and endocrine disruption. Various common foods, including meat, seafood, dairy, grains, and produce, can contain PFAS. Tests on several brands' food packaging have shown elevated PFAS levels. Consuming contaminated foods exposes individuals to potentially harmful levels of these chemicals. Cooking with contaminated water can also be a significant source of exposure to PFAS in food. Both tap water and some bottled waters have been found to contain potentially dangerous levels of forever chemicals Find out more on: https://www.consumernotice.org/environmental/water-contamination/pfas/food/ https://www.consumernotice.org/environmental/water-contamination/pfas/products/ Thank you for reading my blog and I encourage more of my readers to interact with my blogs.
0 Comments
Functional medicine focuses on global health by emphasizing the personalized and systems-oriented approach found in the functional medicine matrix. At the heart of this is the consideration of everyone as a “biochemically individual” patient. Just what does this mean? Definition of “Biochemical Individuality” This term represents the concept that the human body is a composite of each individual's physiological structure, nutritional, and chemical makeup as influenced by their environment, lifestyle, and genes. Some geneticists say we control 80% – 97% of our genetic expressions. Genes are turned on and off by nutrition and the environment. The term was coined in 1956 by Dr. Roger Williams, so it is not a new concept, just a newly used concept. It is a familiar concept in integrative medicine, but not so much in allopathic approaches such as obtained with traditional medical doctors who have had no osteopathic or integrative experience. Functions of Biochemical Individuality in Functional Medicine This term explains how the body individually reacts to stimuli such as:
The most accurate test to determine the nutritional status of the blood is not always a blood test. A “challenge” test or other more specific tests are often needed to determine individuality. For example, a simple blood test of B12 levels may show values in a normal range, but testing for antibodies to vitamin B12 may uncover a problem that otherwise would not be seen. Antibodies against B12 mean you may have adequate B12 levels in the blood, but you also have substances causing the B12 not to work. In addition, folate and B12 should be measured at the same time because deficiencies of both can cause similar symptoms. The Schillings test tells the practitioner if you are absorbing that average level of B12 properly. The methylmalonic test detects early B12 deficiency that a regular blood test would not pick up. These are tests that an MD is unfamiliar with, but that shed light on the intricacies of precise deficiencies and how to fix them. Gene-Nutrient Interactions Each of us may have a unique “barcode” that separates us as individuals buried in our genes. The mind, emotions, behavior, and physiological functioning are all determined to a great extent by the interaction of this “barcode” with nutrition. For example, metabolic syndrome progression largely depends on gene/nutrition/environment interactions. The importance of nutrition cannot be overstated. Studies have shown that personalized dietary instruction improves insulin sensitivity in those with metabolic syndrome, a disease for which no one treatment is entirely adequate. This raises questions about the adequacy of the Recommended Dietary Intake (RDI) levels established by the government and based on “normal” people. The RDI levels did not consider biochemical individuality. Genetotrophic Disease These diseases result from genetically determined metabolic needs not being met through diet and supplements. Medications, the environment, or other nutritional factors may have altered the genes. Nevertheless, the disease will develop if the nutrient in question is not provided. Remember, your doctor does not usually test the vitamin status of your blood, yet these tests are available and are often ordered by dietitians or integrative medicine practitioners. Insurance may cover these tests if properly coded and ordered by a licensed professional such as a Physician's Assistant or Doctor of Osteopathic Medicine. Companies such as Labcorp, or Ulta Labs perform micronutrient tests. *Note: RDs may be able to order reimbursable labs once our licensure is in place next year in 2025. We can already order clinical diets in hospitals and long-term care. Application Consideration of each person's biochemical individuality is integral to a comprehensive functional medicine assessment. Implementing patient-specific treatment plans based on biochemical individuality is essential to the success of patient outcomes. Clinical nutrition used within the contextual framework of Functional Medicine (FM) is similar in structure, but not theory, to Medical Nutrition Therapy (MNT) practiced by registered dietitians as commissioned by the Academy of Nutrition and Dietetics (AND). The difference lies in the theory and how the framework is applied to the individual, where MNT is expanded to operate out of the Functional Medicine Matrix of assessment and treatment.
What is Medical Nutrition Therapy in Functional Medicine? MNT is a clinically focused approach with a defined system of assessment charting and intervention, evaluation, and follow-up considerations. The acronym for this system is ADIME, assessment, diagnosis, intervention, monitoring, and evaluation, and often forms the basis for charting notes. Assessment In functional medicine, the assessment phase differs for clinical nutrition from that of a traditional dietitian or practitioner. In the assessment phase, the probing for information and the tests are clinically specific, and the information is globally pertinent in the areas of environment, society, culture, relationships, stress, sleep, anxiety, eating disorders, food/medication interactions, and work. All this information is considered in the nutrition assessment phase of the FM practitioner as opposed to a pure nutrition assessment of calorie intake, food preferences, and medical history. While the traditional dietitian asks for general labs, the FM practitioner may ask for more biochemical absorption and metabolism tests, such as the Shillings test for B12 absorption or a urinary iodine test for thyroid function. Diagnosis Clinical nutrition diagnoses are biochemically individual based on specific laboratory tests and the functional medicine matrix assessment. Intervention The interventions for an FM clinical nutrition patient may contain elements gathered from the FM matrix and may often include stress interventions to lower cortisol, which affects carbohydrate metabolism, or sleep interventions that affect appetite control during the day. Monitoring After an intervention, one of the most frequent problems is the loss of patients to follow-up. Nutritional therapies must be monitored as many are short-term, and lab reassessments are needed to determine progress and future treatment. For example, a person with high cholesterol/triglycerides may be placed on a low-fat, low-carbohydrate diet with Berberine 500 mg 3x/day for six weeks. Then, a total cholesterol \triglyceride redraw is done to see if progress is being made to determine if berberine needs to be continued or the diet tweaked. Follow-up Follow-up is similar to monitoring, but you are making specific scheduled visits to obtain monitoring data, so the patient expects to come back to see the practitioner on a given date and time. It stresses accountability for the intervention. Goals of Clinical Nutrition in Functional Medicine The goals of clinical nutrition are to use the MNT model in such a manner that:
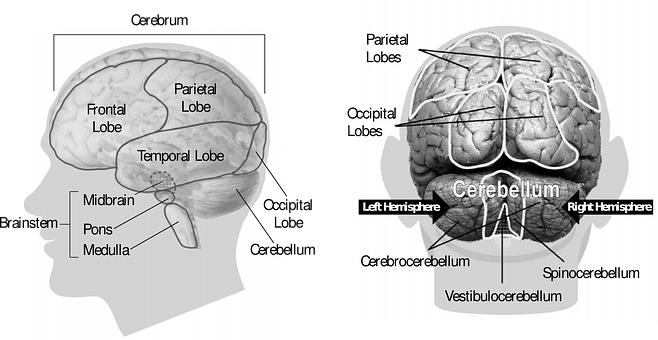
Clinical nutrition is essentially MNT applied within the Functional Medicine Matrix, which customizes all assessments and interventions to personalize the individual's care. It is a comprehensive approach to nutritional intervention that goes deeper yet is more expansive than traditional medicine. Nootropic adaptogens enhance the “state of nonspecific resistance” to stress, a physiological condition linked with various disorders of the neuroendocrine-immune system. Adaptogens exhibit neuroprotective, anti-fatigue, antidepressive, anxiolytic, nootropic, and CNS-stimulating active properties. Notice nootropic effects. Nootropic specifically refers to the actions of the adaptogens that stimulate memory, learning, and overall cognition.
How does one “bio-hack” with nootropic adaptogens? Bio-hacking refers to hacking into the body’s neuro-immune system with those adaptogens known most for their nootropic effects. This creates a sharper memory, bigger brainpower, and maybe even a reversal of mild cognitive impairment or MCI, affecting over 20% of the population. Furthermore, chronic stress is known to compromise brain function in those already suffering from MCI and to be a risk factor for its development. About 284 million people suffer from anxiety disorders worldwide. Given the need for stress relief, scientists have begun studying adaptogens more acutely. Nootropics are of specific interest, given the need for sharper brain power and ammunition against MCI. Most Commonly Used Herbal Nootropic Adaptogens
The most widely studied effect of nootropic adaptogens has been their notorious stabilizing effect on the cortisol hormones, raising them or lowering them as needed. Since cortisol plays a vital role in cognition, keeping the levels regular is important in maintaining a good memory. Other than this effect, numerous other effects can be attributed to this class of plant medicinal, such as:
This is a very new field in conventional medicine, and studies on the use of these agents in the field of mental health are evolving. Ginseng, for example, has been recently proven to enhance cognition in Alzheimer’s disease. However, the widespread use of nootropics for general mental acuity has been utilized for centuries in both Chinese and Ayurvedic medicines. Theoretically, nootropics can prevent or reverse MCI. Since adaptogens also act as nootropics, using an adaptogen to facilitate optimal cognition or reverse MCI is a strategic approach to decreasing stress-related changes that facilitate MCI and optimize existing cognition. Conclusions may be that nootropics be regarded as a novel pharmacological category of anti-fatigue drugs that:
If you feel you need a cognitive bio-hack, choose one of the most commonly used nootropic adaptogens and, with the help of your clinician, design a mental health improvement plan. Dosages for each nootropic differ according to the herbal type (root, powder, tincture) and classification. The inflammatory process is designed to help us with the function and repair of injury. However, inflammation that is out of control and chronic can lead to diseases such as metabolic syndrome or arthritis. Acute inflammation can be downright painful. It is no wonder we have developed anti-inflammatory medications to control these effects and have now turned to a more natural relief, cannabidiol.
What is Inflammation? nflammation is the body’s response to injury. It is the body’s way of telling the immune system that it needs to heal itself, repair damaged tissue, and defend against pathological invaders such as bacteria and viruses. For example, in acute injury, inflammation is usually short, and it is designed to remove the harmful agent. This is a positive inflammatory response. Our job is to prevent the inflammation from getting out of control by taking anti-inflammatory measures. Short-term measures for acute inflammation might include rest, ice, compression, elevation, and topical CBD. When inflammation is prolonged past the critical stage and becomes chronic, tissue damage can occur, and pain can become relentless. What happens when inflammation sets in? Your body increases its production of white blood cells and cytokines to help fight infection. Cytokines are small messenger proteins that can stimulate inflammation. Cytokines can be pro-inflammatory and cause swelling and heat in the tissues as an inflammatory response. Cytokines are also involved in the sensation of pain. CBD has been shown to downregulate cytokines. The primary problem with inflammation is the increased production of free radicals, causing oxidative stress. Oxidative stress is the balance between the production of free radicals and the presence of antioxidants. When there are more free radicals than antioxidants, the body becomes stressed and out of balance, and tissue damage occurs in general. When oxidative stress operates, total speed damage occurs to proteins, fats, and genetic material, specifically. CBD has been shown to have potent antioxidant activity. Signs of inflammation include:
If inflammation is necessary for our body to heal, what types of inflammation do we need to control to feel well and still be in balance and healthy? Acute inflammation Inflammation can be divided into acute and chronic. There is local vasodilation, increased capillary perfusion, accumulation of fluid, and pain from increased cytokine production in acute inflammation.” If these processes are not halted, such as by the use of CBD, and whatever caused the inflammation is not removed, progression to chronic inflammation will occur, which is characterized by a maladaptive immune system and the overexpression of pro-inflammatory genes, the dysregulation of cellular signaling and the loss of barrier function. Examples of acute inflammation:
A reaction to an acute injury will begin within two hours of the injury, and anti-inflammatory measures are generally begun to prevent the inflammation from causing tissue damage or pain from the resulting swelling. Acute inflammation can serve a positive role if it stops an infection from causing tissue damage or cushions an injured joint from further harm. Chronic inflammation is a maladapted immune system response of the immune, nervous, endocrine, and reproductive systems to a perceived threat or injury. This maladaptation leads to such diseases as:
Can CBD be Used for Inflammation? Some of these chronic conditions do not have acceptable treatments for the pain associated with them, such as osteoarthritis. Opioids and non-steroidal anti-inflammatories often do not adequately control the pain and/or are not acceptable as a treatment option. In a landscape of opioid addiction, other viable pain relievers must be found. This is where CBD can be safely used topically or orally to control the pain from the inflammatory process. CBD as a Safe Alternative Anti-inflammatory Current therapies for inflammation involve pharmaceutical drugs with well-known and mostly adverse side-effect risk profiles not only on the cardiovascular system but also on the gastrointestinal tract. Drugs such as diclofenac sodium or ibuprofen are common pharmaceutical answers to inflammation, but they come at a price that may put your heart or gut at risk. CBD has few to no adverse side effects making it a perfect alternative to more dangerous therapies. Does CBD Help With Inflammation? CBD is well known for its anti-inflammatory effects, and CBD limits the formation of free radicals and modulates the function of the immune system. How does it do this? CBD is known to: ● Increase cellular apoptosis (cellular death). Cell death refers to leakage of cell contents into the adjacent tissues, resulting in the transfer of white blood cells to the injured tissue. The accumulation of white blood cells and enzymes and oxygen radicals release enhances the inflammatory reaction. ● Inhibit cell proliferation. The cellular division increases rapidly during the inflammatory process, and CBD slows down the growth of unruly cells. ● Inhibit cytokine production. Cytokines are signaling molecules released from immune cells that cause inflammation. ● Stimulates induction of T-regulatory cells. T-regulatory cells prevent auto-immune disease, are immunosuppressive, and promote wound healing. ● IL-6 suppression IL-6 has pro-inflammatory characteristics and plays a pathological role in autoimmunity and chronic inflammation. CBD amplifies CB2 receptor signaling, which regulates inflammation and immune cell activity. It does this without actually binding to the CB2 receptor, and CBD can down-regulate the CB1 receptor while up-regulating the CB2 receptor. It does this through a myriad of parallel metabolic pathways involving other receptor sites and enzymatic actions. Its actions are often termed the “entourage effect” since CBD works in concert with terpenes, flavonoids and other synergistic molecules to achieve its anti-inflammatory effect. CBD is also known to inhibit a specific enzyme (FAAH) that breaks down the body’s own endocannabinoid, Anandamide, causing these levels to be elevated exerting another synergistic anti-inflammatory effect. CBD Dosage for Inflammation Clinical trials are fervently underway to answer the myriad of questions the new legal status of CBD has ushered in. With CBD status now primarily legal in the US and Europe and the rest of the world taking a renewed interest in it pharmacologically, studies that can accurately answer CBD dosage questions are underway. For now, we have a plethora of animal studies that cannot be extrapolated to humans and small, poorly designed human trials from which to glean some information on dosages for inflammation. Topical doses of CBD for inflammation Animal studies have shown us that low doses of CBD do not exert an anti-inflammatory effect that we must turn to higher doses to achieve local effects. This could be because CBD will interact with cannabinoid receptors in the epidermis (the outer layer of skin tissue) but not enter the endocannabinoid system itself. The epidermis has cannabinoid receptors, but the effect is local, not systemic, which is why topicals can be used without the CBD getting into the bloodstream and, thus, the entire endocannabinoid system. Transdermal applications have shown a dose-dependent response, with the higher doses giving greater pain relief. Animal studies showed a wide range of effective doses from 6.2 – 62 mg/day. Transdermal applications enter the endocannabinoid system. Oral doses of CBD for inflammation Oral bioavailability is quite low – about 13%-19% of the ingested amount. According to one study, suggested oral amounts are 5-25 mg/kg/day. To get an idea how much CBD oil this would be for anti-inflammation for this woman, calculate: for a 60 kg woman, take 60 kg and multiply by 5mg = 300 mg of CBD. The low oral bioavailability is due to the excretion of metabolites via the kidneys and the multiple metabolic pathways CBD undergoes in the transition from the gastrointestinal tract through the liver and then undergoing elimination. Oral CBD bioavailability can be increased if taken sublingually and held under the tongue putting the oil in direct contact with the blood vessel located on the underside of the tongue. Hold the oil there for 60-90 seconds. CBD doses based on weight Other resources based on body weight suggest a dose range of 1-6 mg of CBD per 10 lbs. Of body weight. The weight guideline is unclear on whether these dosage recommendations are for inhaled or oil-based products. For example, starting at the lowest dose of 1 mg per 10 lbs., a 100 lb. woman would need 100 lbs. divided by 10 = 10 x 1 mg = 10 mg to start. Dosages will vary according to several variables, including sex, genetics, environment, presence of food, the form of CBD, age, and others. A scientific basis for the weight guidelines is not found and varies from website to website. What about CBD vaping for inflammation? Doses by inhalation would theoretically be lower as you don’t have to deal with the first pass metabolism associated with digestion and the CBD would pass into the bloodstream within minutes. Clinical data on inhalation doses for inflammation are currently lacking, although a proposal for an aerosol delivery system of 4 mg -200 mg of CBD has been proposed. Is CBD legal for athletes to take for their injuries? All cannabinoids except for CBD are prohibited from the World Anti-Doping Agency (WADA), so CBD is in the clear for using topically or orally to treat inflammatory conditions resulting from sports trauma or injuries. Topical ointments and creams packed with CBD are widely available in doses up to 3500 mg for application on injured areas to subdue pain and reduce swelling in the injured athlete. These may be used in conjunction with CBD oils for a synergistic effect. Application We know CBD works for inflammation, and it offers a safer alternative than opioids or NSAIDs. Many products for CBD treatment exist, and more are being put on the patent market every day. The literature supports using both topical and oral CBD for inflammation, with dosages yet to be determined. Acute inflammation would benefit from topical use of the creams and lotions with supportive oral use as prevention for a few days. More chronic conditions might want to consider oral or aerosol/inhalation devices for use every day to prevent the persistent discomfort prevalent with the pain these inflammatory dysfunctions often bring. And, always, if in doubt, consult your physician or health provider for guidance. Many patients with chronic diseases ask themselves and their doctors this question. The truth is, it is all individual. With some people and some diseases, cures do exist, and with others, they are only managed until a cure can be found or the right therapy implemented.
What is the Difference Between a Cure and Management? A cure entails that all aspects of the disease process are gone, and they aren’t expected to return. Management of a disease is the mainstay of medicine, and its primary function is to control symptoms while the original disease continues to ravage the body. Allopathic medicine, or traditional medicine, uses prescription drugs, topicals, and treatments to help manage bothersome symptoms while often looking for a cure. An example of a typical cure would be athlete’s foot, where the use of topical antifungal creams can get rid of the fungus, and the foot is cured of the infection. Other diseases have no cure, such as pancreatic deficiencies that cause diabetes. While treatments exist to control the blood sugar and ravages of the disease, there is no viable cure for this type of diabetes yet. When is Cure and Management at a Point of Disagreement in Medicine?Philosophies in medicine vary. Allopathic medicine is compartmentalized into a vast array of specialties, making it difficult for a practitioner to see the whole picture and how one system may relate to another when planning a treatment regimen. This also makes it more difficult to find a cure as opposed to symptom management. How often have you gone to the doctor for a simple problem only to be referred to a specialist who never asks you about other dimensions in your life that may be affecting your condition? After all, the doctor is a specialist and only focuses on his specialty. Thus, a specialist manages care but rarely cures the problem. Take hypothyroidism, for example. An endocrinologist will more than likely do a thyroid panel and, if awry, prescribe the appropriate medications to manage the symptoms. There will be no inquiry into whether the hypothyroidism is caused by iodine or selenium deficiency or both. Either deficiency, when treated, may cure hypothyroidism, but a focus on management means the origin of the problem is missed, and the patient continues to be a silent sufferer of a chronic condition that could have easily been cured. Grammar Often Leads to Confusion Cure implies there is a certainty that a medical condition will not be present after a medical intervention. However, many medical conditions have no cure, such as HIV, and management is the only option. Treatment involves examining the processes underlying the risks contributing to the medical condition. Cure involves certainty, and treatment is a process. A process can lead to a cure, but management does not lead to a cure. It only leads to managing symptoms with the underlying cause unidentified. So, when looking for a cure, you aren’t looking to manage your disease; you are looking for a practitioner, of whatever philosophy, be it allopathic, functional, or integrative, that will look at you as a whole person. A person that will not just manage your care but will get to know you as an individual and the variables that might contribute to your chronic illness. Thus, a comprehensive treatment plan is needed to get to the root cause of the problem and promote healing. Take Home Know when your care is only being managed and when you should look for someone who can cure your condition. Too many people settle for managed care when it is within the powers of the individual and the medical practitioner to guide the individual patient to a cure for their illness. Whether it is lifestyle change, taking supplements, or researching the literature, answers to healing many diseases are often within our reach, we just need to cooperate with and seek out those practitioners who look at a condition holistically and keep up to date with the scientific literature. With other conditions, we need to settle for management of symptoms. As with arthritis and heart disease, these chronic conditions have no cure yet, only symptom management and we need to recognize the difference. Even symptom management should be done holistically with a comprehensive treatment plan done by a practitioner who considers the whole picture. The endocannabinoid system, or ECS, is a complex system of cellular signaling present in all vertebrate animals and necessary for our very survival. Discovered in the 1990s while researchers were exploring THC, a well-known cannabinoid present in marijuana, the ECS is now known to be involved in several other physiological systems related to mood, stress, appetite, memory, reproduction, inflammation, sleep, pain, thermogenesis, heart function, and anxiety. Endo, meaning “in” is an important deviation from the word cannabinoid because It implies that these cannabinoids are made within the body and not obtained exogenously from a plant. Essentially, the ECS keeps everything in balance. If you start to sweat on a hot day, it is the ECS that kicks in monitoring your internal environmental temperature and stimulates the sweating or cooling down process. It is responsible for homeostasis in the body. The endocannabinoid system, with its complex actions in our nervous system, immune system and various biological and behavioral systems, it is literally a bridge between body and mind. By understanding this system, we can begin to explore how states of consciousness can affect health or disease. Furthermore, recent research shows that endocannabinoids, phytocannabinoids and the ECS induce widespread or gene specific changes with the possibility of genetic transferability of changes from one generation to the next. This puts a sense of permanency to changes that occur because of the ECS. The ECS Tone The ECS operates in a continuous cascade of enzymatically orchestrated pathways of which the endocannabinoids flow, attach to receptors, are degraded and synthesized as needed. This may all happen congruently in a multi-system fashion. This is called the ECS tone. ECS tone is an indication of the overall state of your ECS. Obesity, for example, represents an elevated hypothalamic endocannabinoid tone. Diabetes is another example of a dysregulated tone. The tone is the overall action generated by the receptors, endocannabinoids, and enzymes all working in sync throughout the body, creating a rhythmic flow that leads to balance in the body. A lack of balance often involves a dysfunctional ECS. How Does the ECS Work?The ECS system is a vibrant and alive system whether you are aware of its processes or not. Endocannabinoids are produced within the body which is why we have receptors for them located in all our major organ systems. Cannabinoid receptors sit on the outside of cell monitoring for conditions both inside and outside the cellular wall to observe changes in cellular activity. Enzymes then respond to changes in cellular activity by degrading the endocannabinoids no longer needed. When signals are received at the receptor that an endocannabinoid is needed, it is made immediately and secreted to attach to the cannabinoid receptor where it is then taken up into the cell and tells the cell how to secrete other substances like hormones or neurotransmitters such as serotonin. They affect how other messages are sent, received and processed by other cells. There are three major components to the ECS system.
Taken together, these three components of the ECS regulatory system ensure that the body remains in homeostasis with neither deficiency nor excess of activity. What Are the Two Main Cannabinoid Receptors?Scientists estimate that the endocannabinoid system evolved over 600 million years ago. Cannabinoid receptors are present throughout the body and are considered to be the most numerous receptor system. Endocannabinoids are cannabinoids our body makes that bind to these receptors, and phytocannabinoids are plant cannabinoids that also bind to these receptors. The two main cannabinoid receptors most studied are CB1 and CB2. CB1 is the most abundant receptor in the brain, while CB2 receptors are found outside of the nervous system, such as in immune cells. The receptors act as a doorway for the cannabinoids to enter the cell. Both endocannabinoids and cannabinoids from plants can bind to the CB1 and CB2 receptors. Receptors are like locks, and THC is like a key that unlocks the door and allows metabolic processes to occur. Both endocannabinoids bind to these receptors like THC does to CB1 but are produced on demand in nerve cells and travel backward to inhibit the release of various neurotransmitters. For example, glutamate is one of the stimulatory neurotransmitters, but when present in excessive concentrations, such as after a stroke or head injury, it can cause neuropathic pain. The endocannabinoids are naturally secreted after such an injury and act to inhibit glutamate release, thus alleviating neuropathic pain. A third receptor, TRPV1 or transient receptor potential vanilloid-one, is also considered part of the ECS and targets the body’s two main endocannabinoids but not THC. Growing evidence shows that non-retrograde communication exists within the ECS. Multiple points of interaction have been identified in the ECS involving the TRPV1 receptor. Evidence points to CBD acting via the TRPV1 receptor in mediating some of its effects in potentially alleviating the inflammation of arthritis. What Are the Two Major Endocannabinoids? Unlike THC, endocannabinoids are produced within the body and bind to the CB1 and CB2 receptors. These two endocannabinoids are: · Anandamide (from Sanskrit meaning “eternal bliss”) · 2-arachidonoylglycerol (2-AG) A unique and striking feature of these endocannabinoids is that their precursors are present in fatty membranes. Upon demand, endocannabinoids are liberated in one or two rapid enzymatic steps and released into the extracellular space. This is in direct contrast to typical neurotransmitters like serotonin which are secreted ahead of time. The routes of synthesis and degradation of anandamide and 2-AG are distinctly different from each other. Relationship Between THC and Endocannabinoids These endocannabinoids are not mind-altering, addictive chemicals such as THC. That is where so much of the public confusion comes in. THC may be similar in structure to anandamide; however, it is not the only plant-based cannabinoid being studied as having effects in the ECS system. Relationship Between THC and CBD Cannabidiol, or CBD, is another cannabinoid under study that does not have the psychoactive effects associated with the plant-based cannabinoid THC. Cannabinoids are compounds found in the cannabis Sativa plant, of which THC and CBD are the most actively studied cannabinoids to date. CBD is the second most abundant cannabinoid after THC in the cannabis plant. In addition, a total of 8 other major ones have been identified, with a total of over 100 confirmed to date. How Do Endocannabinoids Work?Endocannabinoid release occurs immediately after bodily biosynthesis with no intermediate storage for “later use,” making them ideal homeostatic modulators in real-time. This is seen, for example, in appetite regulation. Endocannabinoids regulate appetite and food intake through stimulation of the CB1 receptors, which stimulate the release of hunger/satiety hormones. This all happens relatively rapidly with little thought; it is just an occurrence of “balance” between hunger and satiety. Homeostasis. Balance. The role of enzymes Metabolic enzymes that break down the endocannabinoids after they are used are important for maintaining homeostasis. Two primary enzymes have been isolated that are charged with this duty: · Fatty acid amide hydrolase or FAAH · Monoacylglycerol acid lipase (MAGL) FAAH breaks down anandamide, and MAGL breaks down 2-AG. These enzymes guarantee that endocannabinoids are used for as long as needed and no longer. This is a distinguishing factor of these enzymes from the actions of hormones or other regulating signals like neurotransmitters, which can persist for seconds or minutes or be packaged and stored for later use. These enzymes cannot break down plant-based cannabinoids, a limiting factor in cannabinoid research relative to disease treatment. This means that if an active dose of cannabinoids is found for an illness, the exact dosage must be determined because the natural homeostatic mechanisms of the ECS will not be able to regulate cannabinoids administered from the plant. Endocannabinoid Deficiency As we learn more about the ECS, we discover diseases that may be classified as endocannabinoid deficiency diseases. Medical science has termed these clinical endocannabinoid deficiency dysregulation diseases, or CECD for short. The available evidence seems to indicate that the ECS systems suffer from a deficiency of anandamide, thus suggesting that treatment of the ECS to upregulate the tone might benefit these disorders. These conditions include:
The conditions listed frequently involve more than one physiological system and effective treatment for them has been difficult to unearth. It is only logical that science would look to multisystem treatment modalities such as cannabis to treat multisystem disorders such as the ones just mentioned. How Does THC Interact With the ECS? THC interacts with ECS in the same manner as the endocannabinoids do. It can bind to either CB1 or CB2 receptors and is not subject to enzymatic regulation, thus the problem with addiction and mind alteration. On the other hand, it may help with pain and stimulate the appetite of those who have lost theirs, as in cases of anorexia. How Does CBD Interact With the ECS? CBD is a different story. CBD doesn’t make you “high” and doesn’t carry any negative side effects such as paranoia or delusions. Experts don’t exactly agree on how CBD works or even exactly what it does, but they hypothesize that it prevents endocannabinoids from being broken down through the effects of the enzymes. Scientists do know that CBD doesn’t bind to the CB1 or CB2 receptors in the same manner as THC. Science has proven that CBD prevents the enzyme FAAH from breaking down cannabinoids, unlike THC, where enzymes have no effect. The ECS is the key to maintaining homeostasis in our body. It may one day hold the answers to treatments for diseases that affect multiple organ systems for which we have no treatments. The ECS offers a rich landmine of untapped research and potential therapeutic applications. Concluding Remarks We need to further educate others on the important role of the ECS on cannabinoids and the differences between THC and CBD. Along with more research, we need to keep an open mind as to the application of cannabinoids to therapeutic treatments of multi-system disorders for which we currently have no well-defined treatment protocols. And keep in mind that lifestyle activities can alter endocannabinoid tone and, thus, ECS activity. Research has shown that diet, supplements, herbs, weight control, and exercise also modulate the ECS tone. Clinical trials investigating these modalities are sorely lacking and in need of attention. In conclusion, the ECS may be a newly discovered system, but it is old in its presence and seemingly imperative to our existence. Furthermore, the field of pharmacology is now considering all members of the ECS as potential novel therapeutic targets for the modulation of problematic diseases. The discovery of the ECS opened a doorway to the discovery of possible novel therapeutic agents that can be utilized in the form of cannabinoids or related chemical structures to modulate health and disease without the adverse side effects so often associated with the psychoactive cannabinoid THC. Keywords: endocannabinoid system, anandamide, 2-AG, ECS, endocannabinoid deficiency, cannabinoid receptors Berberine is a chemical found in several plants, including European barberry, goldenseal, goldthread, Oregon grape, philodendron, and tree turmeric. It belongs to a class of compounds called alkaloids. It is said to have powerful effects similar to pharmacological and has been used for centuries in Chinese medicine. It is just now coming of age in modern nutritional medicine to treat diseases such as diabetes.
How Does Berberine Work? Berberine is known to stimulate insulin secretion and activate AMPK, an enzyme known to regulate cellular energy metabolism. Its primary actions are to:
Effectiveness of Berberine in Diabetic Patients Berberine has been found to act similarly to the commonly used diabetes drug Metformin. It is not clear whether metformin and berberine undertake all actions via the same mechanisms or some via similar and other different mechanisms. While the severe adverse gastrointestinal side-effects that interfere with metformin compliance are generally absent in berberine treatment — berberine and metformin (or other oral hypoglycemics) treatment has been superior in controlling glucose than either treatment alone. Dosage Dosage and treatment duration may vary with the patient’s age. Data suggests that berberine therapy becomes unremarkable in treatments lasting more than 90 days or in amounts greater than 2 grams. Further clinical studies of longer duration are needed in this area. The most effective dose is 500 mg three times a day. Because most anti-diabetic drugs cannot be used in patients with hepatic dysfunction, renal disease, and heart disease, this makes pharmacological therapy of type 2 diabetes complicated — and the use of other nutraceuticals such as berberine more desirable. Current studies have reported the significance of berberine against oxidative stress and inflammation in cells, elaborating on its vital role in diabetes mellitus. Generally, a decrease in blood glucose level by 20%–40% is reported in fasting patients treated with berberine alone; this effect resembles that of rosiglitazone and metformin treatment. Application Preliminary research from animal and human studies indicates that berberine therapy in dosages of 500 mg three times per day may be an advantageous treatment for type 2 diabetes. This effect occurs alone or in conjunction with other hypoglycemics for optimal blood sugar control with minimal adverse side effects. Berberine's mechanisms of action mirror those of the common anti-diabetic drug metformin, but it does not have the side effect of severe diarrhea associated with metformin. Further long-term studies are needed on human subjects to identify the exact mechanisms of action and duration of treatment best utilized for long-term blood sugar control of diabetes. The blame for the obesity epidemic has been placed on everything from genetics to poor eating . . . but is there a darker, unspoken human need that remains unfulfilled and often even unknown even to oneself? Let’s start this part of our transformative inquiry by being honest with ourselves, confronting the sabotages, finding ourselves, and then not losing that person again.
Unmet emotional (and spiritual) longings are recurrently filled by food, yet the longing and emptiness remain. Our mind, in its ultimate judgment, feels empty, lonely, starved for affection or belonging recurrently and unconsciously, even telling our bodies to turn to food to gain some feeling of being “full.” Food eventually becomes a learned substitution for every need in our lives, including how to deal with stress, loss, grief, loneliness, and loss of faith. Stress alone comes with its own sad story of fat hormones and carbohydrate intolerance, which may lead to sleep issues. Lack of adequate sleep, in turn, contributes to “fatness.” Constantly, almost like a mouse on a wheel, we try and try but get nowhere. Miraculously, if goals are met, the weight is lost – think . . . just how permanent is it? Usually, not very. It is because the elephant in the room, our heart, our soul, is still in the room unattended, unfulfilled, and even unrecognized. Is it feasible to expect that with growing awareness of these other barriers to long-term weight-loss success, a separate treatment plan would blossom out of a need for permanent wellness success? Oh, Where to Begin to Find Such Secrets to Be Solved? Both the logical and exercise science points of view determine that obesity is caused by energy input being greater than energy output. Many people’s palates and brains are addicted to high salt, sugar, and fatty food, true. This notion is also consistent with science, but I believe other etiologies with more effective approaches are out there but underutilized, as just discussed. Humans are emotional creatures, and there is no denying basic instincts such as finding community, love, pleasure, and happiness. Unlike our land and sea mammals, which are driven biologically to reproduce and survive, humans have an expansive consciousness with the free will to choose how they want to live. The gift of choice without knowledge sometimes harms our overall balance and well-being. It can be argued that over the years, families have changed, giving birth to an entire generation with prominent negative health behaviors. If a child grows up eating fast food and drinking soda in replacement for water, the child will grow up into an adult who passes these behaviors and unhealthy ways of coping down to his/her family. Simply put, what science and psychology say about obesity is true, and an integrative approach to this problem must be taken globally. No longer can feelings, anger, stress, sexual dysfunctions in marriages or relationships/break-ups – no longer can they be ignored and swept under the rug. The underlying causes of obesity are driven by emotions, which then become akin to an addiction caused by the release of hormones and neurotransmitters in the body. Many food chemists, for example, design food to become addictive, which plays into the role of overeating. It’s a vicious cycle that takes time to retrain the body and brain. This is a huge job and one that is not being done in its entirety in any weight loss program today. Plan For Listening to the Inner Self, Your Emotions, Your Beliefs For many obese people, they have “lost” their power somewhere on their journey in life. Many keep giving their power away to their boss, spouse, children, friends, or anyone who needs their service. Those who have power but still struggle emotionally are stuck in belief systems that they can’t be or look a certain way. This, too, is linked subconsciously to being powerless. Many experience the domino effect. Sometimes it starts with one scenario that leads into other and more complex situations later in life. Many who have been verbally, physically, or sexually abused in the past are likely to fall into negative eating habits. Mostly, with women, there is either an underlying sense of shame or the need to be unattractive to men. I have found this with women who were sexually abused in their upbringing. In fact, they cover and hide any sense of beauty and love that can shine from their power center. People are obese for many reasons, but those who are not emotionally happy often seek fulfillment and validation through overeating. Those who “MUST eat their ice cream every day” have connected a certain food with a certain feeling. Why is this connection to a certain food that important? Questions like these must be asked and answered with a plan for emotional fulfillment without the use of food. A truly balanced person never has a biological urge to “need” a certain daily food for survival. The most important lesson is that power must be balanced. Those who have excess power often abuse their personal strength. Or they use their power to compensate for something else lacking in their life. Not everybody has emotional problems, but for many, the emotion is deeply buried and allows others to control our lives instead of ourselves. Even if a person is religious, he or she may not be spiritually fulfilled and in control of his or her life, choices, and emotions. Start by listening:
©Kathryn Shattler, Synergetics Weight Loss for Life Plan Hitting a weight loss plateau is typical for any low-calorie meal plan you may be following. It is a notorious roadblock for anyone wanting to lose weight, and the game plan is to succeed on that weight loss plan, be it keto or other. Here are ten reasons why you may be hitting a plateau while trying to follow a keto diet:
What is the best keto diet, you ask? The keto Mediterranean Diet is the healthiest keto diet plan to follow. It has healthy fats that won't clog up your arteries, and it's good for your heart. So, don't give up. Plan for the plateaus! |
Author
|






 RSS Feed
RSS Feed